Hypogonadism and right ventricular failure with testosterone deficiency myopathy
A 30 YEAR OLD WITH BILATERAL PEDAL EDEMA AND DYSPNEA ON EXERTION
FOLLOWING IS THE PROBLEM LIST ACCORDING TO PATIENT'S PRIORITY:
MAIN COMPLAINTS:
1. Bilateral pedal edema
2. Dyspnea on exertion
3. Papitations
4. Decreased urine output
5. Dry Cough
EACH COMPLAINT IN DETAIL:
1.Bilateral pedal edema:
Since 15 days
Upto knees
PROBABLE CAUSE:
- Heart Failure
- Liver disease -- ruled out as there is no ascites
- Malnutrition --ruled out as there is no abdominal distention
- Renal cause --ruled out as there is no facial puffiness
- Thyroid disorder --rare
Since 15 days
Past history: first became breathless on walking for short distance and while going upstairs
There is also a history of nocturnal wheezing
Not associated with orthopnea/PND
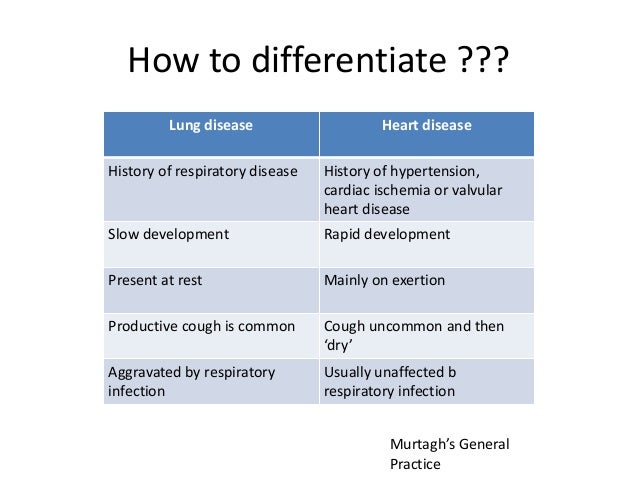
PROBABLE CAUSES:
- Respiratory cause( COPD,Pneumonia)
- Anemia
- Renal cause --ruled out as there is no symptoms like facial edema
- Heart failure
Source: https://www.slideshare.net/muhammadhelmi37853/dyspnoea-respiratory-failure
3. Papitations:
Since 1 year
Persistent, Pounding type
Aggravated by EXERTION
Relieved on REST
POSSIBLE CAUSES:
- Cardiac causes:Mitral valve prolapse,pericarditis,congestive heart failure
- Non-cardiac causes:Hyperthyroidism, hypoglycemia
4.Decreased urine output:
Since 2 days
POSSIBLE CAUSES:
- Dehydration
- Kidney failure
- Heart failure--can lead to renal failure
5.Dry Cough:
Since last 15 days
No expectoration
POSSIBLE CAUSES:
- Allergic rhinitis -- ruled out as there are no symptoms like sneezing and runny nose and so no history of allergies
- Pneumothorax --ruled out as there is no pleuritic pain
- Pulmonary embolism -- ruled out as there is no hemoptysis
- Heart failure
No H/O hemoptysis
No increase in frequency in micturition
PAST HISTORY:
- No similar complains in the past
- Not a known case of HTN,Diabetes,EPILEPSY,CVA,CAD
- No similar complaints in the family
- Mixed diet
- Appetite and sleep -- decreased
- No addictions, no allergies
GENERAL EXAMINATION:
- He is consious,coherent and cooperative,moderately built and nourished
- Afebrile
- Pallor absent
- No Icterus,cyanosis,clubbing,lymphadenopathy
- EDEMA: B/L pitting type of pedal edema upto knees
- BP:120/70mmHg
- RR:20cpm
- PR:124bpm
- Undescended testis(cryptochidism)
- Very less facial hair+less pubic hair+no axillary hair=Tanner Stage 4
ON EXAMINATION:
RESPIRATORY SYSTEM
Bilateral air entry +
Normal vesicular breath sounds
CVS
Visible pulsation over Tricuspid and Mitral areas
Apex beat felt over V intercostal space within Midclavicular line -- foreceful and well sustained
Right Ventricular Heave +
JVP raised with prominent 'a' wave
S1, S2 heard with prominent P2
CNS
Conscious, coherent, cooperative, well oriented to time,place and person
High mental functions=Normal
Minimental Score = 28 --> Normal cognition
High-Stepping Gait
MOTOR SYSTEM:
- Bulk, Tone - Normal
- Power: slightly low in Lower limbs>Upper limbs
- Reflexes: Present
- SENSORY SYSTEM:
- Anterolateral and dorsal tract senses - INTACT
- Tactile sensation - NORMAL
- Two point discrimination - IMPAIRED in LOWER LIMBS
- Skull, spine -Normal
- No cerebellar or meningeal signs
ABDOMEN: Normal, bowel sound present
INVESTIGATIONS SHOWED:
T3 levels -- slightly low
FBS levels -- slightly high
ALP levels -- High
Albumin in urine - Present
Low RBC count, hemoglobin, PCV
USG: Raised echogenicity of B/L Kidneys
Colour doppler 2D Echo:
- Valves - Normal
- Right atrium and ventricle -- Dilated
- Inferior vena cava-- Mildly dilated
- Tachycardia
- Mild AR, Moderate TR, Trivial MR
- Good LV systolic function
- No AS/MS, No PAH/PE
- ECG:

- X-Ray:

- USG Scrotum:
- B/L Scrotal sac empty
- Both testes not found in B/L inguinal region
- Prostate - Present
- Urinary bladder - partially distended
ANATOMICAL LOCATION OF THE ROOT CAUSE:
Bilateral Pedal edema is not associated with facial puffiness and no ascites --thus renal cause and hepatic disease ruled out
Dyspnea is on exertion and is associated with dry cough and not associated with orthopnea
Palpitations are pounding type and associated with shortness of breath indicating the cause being the HEART
Dry Cough is not associated with hemoptysis,sneezing,runny nose or H/O hemoptysis -- thus allergic rhinitis and pulmonary embolism can be ruled out
2D ECHO findings:
- Valves - Normal
- Right atrium and ventricle -- Dilated
- Inferior vena cava-- Mildly dilated
- Tachycardia
- Mild AR, Moderate TR, Trivial MR
- Good LV systolic function
- No AS/MS, No PAH/PE
JVP: elevated with prominent 'a' wave --
"There are only two causes of giant a waves: decreased right ventricular compliance or tricuspid stenosis. Causes of the former are pulmonary valve stenosis, chronic obstructive pulmonary disease with associated pulmonary hypertension, or restrictive cardiomyopathy, each of which decreases right ventricular compliance. In these conditions the force of right atrial contraction is increased and generates a giant a wave during atrial systole. As pulmonic valve stenosis and tricuspid stenosis are uncommon diseases in adults, giant a waves almost invariably indicate either pulmonary arterial hypertension or a restrictive cardiomyopathy involving the right ventricle."
Thus, it is most probably RIGHT VENTRICULAR FAILURE.
The right ventricular failure may be primarily due to pulmonary hypertension.
PHYSIOLOGICAL FUNCTIONAL DISABILITY:
According to the source-https://www.verywellhealth.com/symptoms-and -complications-of-heart-failure-4161320
"With heart failure, the pumping of the heart is less efficient than normal. To compensate for this reduced pumping ability the body attempts to hold on to salt and water. The accumulation of sodium and water can initially improve cardiac function, at least marginally—but eventually, fluid accumulation becomes excessive and leads to several kinds of symptoms."
In heart failure, the body’s accumulation of salt and fluid produces increased pressures in the cardiac chambers. Elevated cardiac pressure causes some of that excess fluid to accumulate in the lungs. The result is lung congestion.
This lung congestion typically causes breathing difficulties that can produce several distinct symptoms such as Dyspnea on exertion, Dry cough
:max_bytes(150000):strip_icc():format(webp)/heart-failure-symptoms-5ad8b9bfae9ab80038133c25.png)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5512682/ says--"Testosterone (T) has a number of important effects on the cardiovascular system."
Certain sources say--https://pubmed.ncbi.nlm.nih.gov/29712743/
Hypogonadism can have certain neurological features
Also, decreased testosterone levels can lead to the so called TESTOSTERONE DEFICIENCY MYOPATHY according to a journal-https://www.researchgate.net/publication/15635947_Testosterone_deficiency_myopathy
- Hypogonadism can change the calf muscle elasticity thus causing muscle weakness in the lower limbs--REFERENCE: https://eje.bioscientifica.com/view/journals/eje/156/6/1560673.xml
ETIOPATHOGENESIS:

https://www.sciencedirect.com/science/article/pii/S0735109716369133

https://www.sciencedirect.com/science/article/pii/S0735109713058701
DIAGNOSIS:
Right ventricular failure with primary Pulmonary artery hypertension due to hypogonadism
Hypogonadism (tanner stage 4)
Lower limb proximal myopathy
Oral candidiasis with poor oral hygiene
impaired glucose tolerence
- PHARMACOLOGICAL:
- Tab. Pantop 40 mg po/ OD
- Inj. Lasix 20 mg iv/ BD
- Inj. Thiamine 1amp. in 100 ml NS
- Inj. Optineurin 1amp in 100 ml NS
- Tab sildenafil 10mg po OD
- Tab benformet plus od
- On diuretic therapy and vaso dilator therapy patient got better and discharged in stable condition
- NON-PHARMACOLOGICAL:
- Fluid and salt restriction
- Diet according to Harvard plate
- Primarily, Testosterone hormone replacement therapy and medication for the heart failure may can solve the problem in this patient.
- Fluid (1.5 to 2 L/day) and salt (2 gm /day) restriction
- Tab sildenafil 10 mg po/bd
- Tab benformet po/OD for 2 weeks
- Chlorhexidine oral gargles for two weeks
- Oral candid paint
- Diet according to Harvard plate
- Work up for FSH,LH,GNRH
- Review after 2 weeks
- Davidsons principles of medicine

Hi Shivani. Nicely presented and I can see that you took a genuine interest in analysing this case. There are a few discrepancies in Sai Kiran's blog and I'd suggest you go through Vidya's blog for a slightly different version of the patient's life events. His dyspnea has been there since 8 months now and 15 has been incorrectly posted in Kiran's blog.
ReplyDeleteHere is the link to Vidya's blog
vidya8829.blogspot.com
And yes the patient has a waddling gait and not a high stepping gait.
Please review Vidya's blog and provide further inputs.
Great work.
Sure...i will go through the other blog
ReplyDeleteAnd Thank youu...