The Curious case of ANASARCA
MEDICAL MYSTERY
I've been given these two case datas to solve in an attempt to understand and analyize the topic based on patient clinical data in order to develop competency in reading and comprehending clinical data related to the case and come up with a suitable diagnosis.
CASE 1
45 yr Female with Anasarca
ANSWER TO THE QUESTIONS THAT AROUSE DURING ANALYZING THE CASE ARE:
1) What is your complete anatomic and etiologic diagnosis from the data available in the patient's online record linked above? (ignore the provisional diagnosis on admission mentioned in the case report)
ANATOMIC DIAGNOSIS:
According to the patient's clinical history,
- The defect is likely to be in the kidneys as the patient had pitting type pedal edema,facial puffiness associated with decreaased urine output,SOB even at rest
- Heart failure is ruled out as there is no JVP elevation and symptoms like facial puffiness mainly poitn towards RENAL CAUSE
- The defect in her kidneys may have primarily occured as a long term sequelae of diabetes as she is a known case of DIABETES since 5 yrs, that has led to hypertensive changes in the vessels(H/O hypertension since 1 year) that caused a reduced perfusion to the kidneys leading to reduced kidney function.
- High blood sugar from diabetes progressively damages the kidneys, eventually causing chronic kidney disease.
- Protein in the urine (nephrotic syndrome) may also result.
- Hypertensive nephropathy: Kidney damage caused by high blood pressure.Chronic renal failure may eventually result.
- The RENAL FAILURE in this patient is basically MULTIFACTORIAL.
- The factors are DIABETES, HYPERTENSION, OBESITY and maybe some DRUG TOXICITY as well.
- When diabetes is not well controlled, the sugar level in your blood goes up. This Hyperglycemia (high blood sugar)can cause damage to many parts of your body, especially the kidneys, heart, blood vessels, eyes, feet, nerves.
- Diabetes can harm the kidneys by causing damage to:
- Blood vessels inside your kidneys:The filtering units of the kidney are filled with tiny blood vessels. Over time, high sugar levels in the blood can cause these vessels to become narrow and clogged. Without enough blood, the kidneys become damaged and albumin (a type of protein) passes through these filters and ends up in the urine where it should not be.
- Nerves in your body:Diabetes can also cause damage to the nerves in your body. Nerves carry messages between your brain and all other parts of your body, including your bladder. They let your brain know when your bladder is full. But if the nerves of the bladder are damaged, you may not be able to feel when your bladder is full. The pressure from a full bladder can damage your kidneys.
- Urinary tract:If urine stays in your bladder for a long time, you may get a urinary tract infection. The bacteria causing UTI may grow rapidly in urine with a high sugar level. Most often these infections affect the bladder, but they can sometimes spread to the kidneys.
REFERENCE:
HYPERTENSION AS THE FACTOR:
How are high blood pressure and kidney disease related?
They are related in two ways:
1. High blood pressure is a leading cause of CKD. Over time, high blood pressure can damage blood vessels throughout your body. This can reduce the blood supply to important organs like the kidneys. High blood pressure also damages the tiny filtering units in your kidneys. As a result, the kidneys may stop removing wastes and extra fluid from your blood. The extra fluid in your blood vessels may build up and raise blood pressure even more.
2. High blood pressure can also be a complication of CKD. Your kidneys play a key role in keeping your blood pressure in a healthy range. Diseased kidneys are less able to help regulate blood pressure. As a result, blood pressure increases.
REFERENCE:
https://www.kidney.org/sites/default/files/docs/hbpandckd.pdf

OBESITY AS THE FACTOR:
Extra weight forces the kidneys to work harder and filter wastes above the normal level. Over time, this extra work increases the risk for kidney disease.

REFERENCE: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5433675/
2) What are the reasons for her:
Azotemia:
Azotemia is the elevated levels of urea and other nitrogen compounds in the blood.
It indicates that there is problem with kidneys filtering the nitrogenous compounds
Azotemia is generally the result of renal parenchymal damage which leads to UREMIA later
According to https://emedicine.medscape.com/article/238545-overview#a4 :
"Azotemia occurs in three physiologic stages:
- PRERENAL AZOTEMIA -resulting from problems in the systemic circulation that decrease flow to the kidneys.
- INTRARENAL AZOTEMIA -resulting from problems in the kidney itself.
- POST RENAL AZOTEMIA -resulting from obstruction in the collecting system."
Anemia:
- The reason for anemia in this patient maybe due to iron deficiency due to protein energy malnutrition
- According to-https://www.niddk.nih.gov/health-information/kidney-disease/anemia#:~:text=Healthy%20kidneys%20produce%20a%20hormone%20called%20EPO.,red%20blood%20cells%2C%20causing%20anemia.

Hypoalbuminemia:
"Hypoalbuminemia is common in patients with end-stage renal disease (ESRD). It is caused by a combination of a reduced synthesis and an increased degradation of albumin. The altered albumin homeostasis in ESRD patients is caused by a systemic inflammatory state which correlates closely with mortality. Hypoalbuminemia is a strong predictor of an adverse prognosis, but it is not a pathogenic factor in itself."
Acidosis:
"In patients with chronic kidney disease (CKD), the causes of metabolic acidosis include: impaired ammonia excretion, decreased tubular reabsorption of bicarbonate and insufficient production of bicarbonate in relation to the amount of acids synthesised in the body and ingested with food."
REFERENCE:
https://www.karger.com/Article/FullText/490475#:~:text=In%20patients%20with%20chronic%20kidney%20disease%20(CKD)%2C%20the%20causes,body%20and%20ingested%20with%20food.
3) What was the rationale for her treatment plan detailed day wise in the record?
Particularly mention rationale and efficacy for some of the drugs administered such as oral and iv bicarbonate?
- Inj. NaHCO3 -- it is used to make blood and urine more alkaline and it lleads to reduced protein catabolism, reduced ammonia production, and tubular damage
- Syp. POTCHLOR -- it is given to treat hypokalemia
- Inj. HAI -- to control diabetes
- t.OROFER -- iron therapy for renal anemia
- t.PAN -- to prevent GERD
- Inj. LASIX -- diuretic used to treat fluid overload and acidosis
- t. DYTOR -- DIURETIC used to treat edema
- Telma -- antihypertensive used to lower the blood pressure
- Inj. erythropoietin -- used to treat anemia by stimulating bone marrow to prduce blood cells
- t.nodosis -- oral bicarbonate acting as antacid to relieve acid base disturbances and treat electrolyte disturbances
- t.shelcal -- combination of calcium and vitamin D3 to treat their deficiencies in renal failure.
- syp.lactulose -- to promote fecal excretion of water, sodium, potassium, amonium, urea, creatinine and protons in renal failure
- Protein X powder -- supplementing protein as dialysis was performed
- Inj. MONOCEF -- cephalosporin antibiotic given in dialysis patients to prevent infections
When is iv or oral bicarbonate indicated and why is it contraindicated in certain situations?
Indications:
- IV bicarbonate is a medication primarily used to treat severe metabolic acidosis and used only when pH is <7.1 and when the cause is either diarrhea,vomiting or renal causes.
- Sodium Bicarbonate is indicated in the treatment of metabolic acidosis which may occur in severe renal disease, uncontrolled diabetes, circulatory insufficiency due to shock or severe dehydration, extracorporeal circulation of blood, cardiac arrest and severe primary lactic acidosis.
- Contraindicated in any situation where salt retention is undesirable such as edema,heart disease,cardiac decompensation and primary or secondary aldosteronism.
- Sodium Bicarbonate (sodium bicarbonate 5% injection) Injection is contraindicated in patients with metabolic and respiratory alkalosis and in patients with hypocalcemia in which alkalosis may produce tetany.
- It is also contraindicated in pregnancy due to teratogenecity.
4) What was the indication for dialysing her and what was the crucial factor that led to the decision to dialyze her on the third day of admission?
INDICATION of Dialysis in this patient is SEVERE METABOLIC ACIDOSIS and REFRACTORY ANURIA.
The crucial factor that led to the decision to dialze her on the 3rd day od admission is the worsening of severe metabolic acidosis and SOB and occurence of refractory anuria.
5) What are the other factors other than diabetes and hypertension that led to her current condition?
The factors other than diabetes and hypertension that led to the patient's current condition are:
- Obesity
- Toxicity due drugs like those of pain killers taken by the patient.
6) What are the expected outcomes in this patient? Compare the outcomes of similar patients globally and share your summary with reference links.
According to https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5261605/ -
"Risk factors for the poor outcomes of RF in very elderly patients with AKI were BMI, baseline eGFR, low MAP, low prealbumin level, hypoalbuminemia, oliguria, BUN level, and more severe AKI stage. Identifying risk factors may help to improve patient outcomes."
According to https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2974373/#:~:text=in%20larger%20trials.-,Conclusion,no%20change%20during%20follow%2Dup. --
"Long-term outcome of AKI consists of a high additional mortality unrelated to treatment modality offered during hospitalization, varying evolution of renal recovery, and many comorbidities, but a mental health at the same level as the general population."

ACCORDING TO A STUDY--
"In conclusion, the long-term survival of patients with AKI admitted to the ICU is poor."
"This mortality rate is not related to disease severity or treatment modality offered during hospitalization. Comparison of renal function between discharge and follow-up shows no change during follow-up. A considerable part of the hospital survivors stayed in need of chronic RRT and had important comorbidities. The physical component health-related quality of life of the SF-36 score in the survivors was lower compared with age-matched general populations, whereas the mental health-related quality of life was found to be the same as in the general population."
7) How and when would you evaluate her further for cardio renal HFpEF and what are the mechanisms of HFpEF in diabetic renal failure patients?
EVALUATION:
1.CARDIAC IMAGING STUDIES:
- An echocardiogram is warranted in any CKD patient presenting with new cardiac symptoms or events.
- "For ESRD patients, the kidney disease outcomes quality initiative (KDOQI) guidelines recommend echocardiograms to be performed 1–3 months after the start of dialysis and every 3 years thereafter, regardless of symptoms. Other authors even suggest a closer follow-up, with serial examinations every 12 to 18 months."
- "CKD patients with significant LV systolic dysfunction should undergo an evaluation for coronary artery disease.This may include both noninvasive imaging (stress echocardiography, nuclear imaging, or computed tomographic angiography) and invasive imaging tests (coronary angiography), as recommended by KDOQI guidelines."
- Coronary angiography is indicated in patients presenting with HF and known or suspected coronary artery disease, except for those ineligible for revascularization therapy.
- Instead, computed tomographic angiography may be used in cases with an intermediate likelihood of coronary artery disease; however, this procedure has potential technical limitations in CKD, because of the severity of vascular calcifications, which may reduce the accuracy of coronary imaging .
- Cardiac magnetic resonance imaging (MRI) enables accurate measurements of LV and LA volume and can identify myocardial viability and scar tissue; however, given the issues of cost and availability, as well as the risk of nephrogenic systemic fibrosis from gadolinium contrast in CKD patients, MRI is not currently recommended as a routine imaging test in this population.
2.ASSESSMENT OF FLUID STATUS
- Assessment of fluid status is very important in all CKD and, particularly, ESRD patients. In those with CKD and HF, volume overload may be both a result and a precipitating factor of the latter condition.
- The echocardiographic measurement of inferior vena cava diameter and collapsibility can accurately predict right atrial pressure and volume status in HD patients, and the adjustment of dry weight based on this technique was shown to prevent intradialytic adverse events, to reduce LV mass and LA size, and to improve quality of life.
- Relative plasma volume monitoring is a safe and inexpensive procedure that monitors relative plasma volume by analyzing blood density and allows automatic feedback control of the ultrafiltration rate that prevents relative plasma volume from reaching a critical level. This technique has decreased intradialytic hypotension, and a recent study suggested that it may aid dry weight assessment during HD.
- One of the most promising methods of assessing dry weight that have emerged in recent years is bioelectrical impedance analysis (BIA). This method estimates body composition, including total body water (TBW), extracellular water (ECW), and intracellular water (ICW), by measuring the body’s resistance and reactance to electrical current. It has been validated in healthy subjects and various patient populations by isotope dilution and other body composition techniques. The procedure is safe, simple, and relatively inexpensive.
- Several studies have proved the usefulness of BIA for the evaluation of dry weight in HD patients. Overhydration >15% of ECW as measured by BIA was demonstrated to predict mortality.
- In CKD and ESRD plasma levels of natriuretic peptides are affected by the impaired renal clearance; however, they still maintain a strong relation with LV end-diastolic wall stress.
- In dialysis patients, plasma natriuretic peptides have shown significant associations with LVH, LV systolic and diastolic dysfunction, and LA dilatation.
- Furthermore, it has been demonstrated that BNP and NT-pro-BNP can predict the risk of HF in nondialysis CKD and in PD patients, respectively. These data clearly suggest the potential interest in the use of natriuretic peptides in the diagnosis and management of HF in CKD and ESRD.
MECHANISM OF HFpEF in renal failure patients:
REFERENCE--https://www.sciencedirect.com/science/article/pii/S0085253819302765

According to- https://www.hindawi.com/journals/bmri/2014/937398/
"Abnormalities of left ventricular (LV) structure and function are very common in CKD and ESRD patients. Among ESRD patients, approximately 73.4% of those who are started on dialysis have LVH, 35.8% have LV dilatation, and 14.8% have LV systolic dysfunction"
"A large number of nonhemodynamic factors also contribute to the development of LVH and cardiomyopathy in CKD patients."
"For example,
- Hyperphosphatemia has been associated with high blood pressure (BP), increased LV mass, and diastolic dysfunction.
- Excess angiotensin II can accumulate in the heart and promote myocyte hypertrophy, interstitial fibrosis, and microvascular disease, as well as cardiac conduction disturbances, QT prolongation, and arrhythmias.
- High serum aldosterone, resulting from activation of renin-angiotensin system or other pathways, can induce myocardial fibrosis, possibly by release of transforming growth factor β.
- Sympathetic overactivity, which has been demonstrated in CKD, is also deleterious to the heart and may induce LV concentric remodeling."
8) What are the efficacies over placebo for the available therapeutic options being provided to her for her anemia?
According to a reference study-https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4946860/
"In a study, ferumoxytol was shown to be an efficacious and generally well-tolerated treatment option for patients with IDA and underlying GI disorders who were unable to use or had a history of unsatisfactory oral iron therapy."
"Ferumoxytol-treated patients demonstrated significantly greater improvements in FACIT-Fatigue and various domains of the SF-36 than placebo-treated patients"
9)What is the utility of tools like the CKD-AQ that assess the frequency, severity, and impact on daily activities of symptoms of anemia of CKD?
According to-
"The CKD-AQ is a novel PRO measure that captures the frequency and severity of the most relevant symptoms and impacts associated with anemia of CKD."
"The CKD-AQ captures the frequency and severity of the most relevant symptoms and impacts associated with anemia of CKD. It has the potential to assist clinicians in assessing and understanding patients' symptoms due to anemia of CKD as well as to help evaluate treatments for anemia of CKD in clinical trials."
"Future studies will evaluate its psychometric properties and its potential utility in anemia management."

Is Telegu among the 68 languages in which it is translated?
10) What is the contribution of protein energy malnutrition to her severe hypoalbuminemia?
According to-
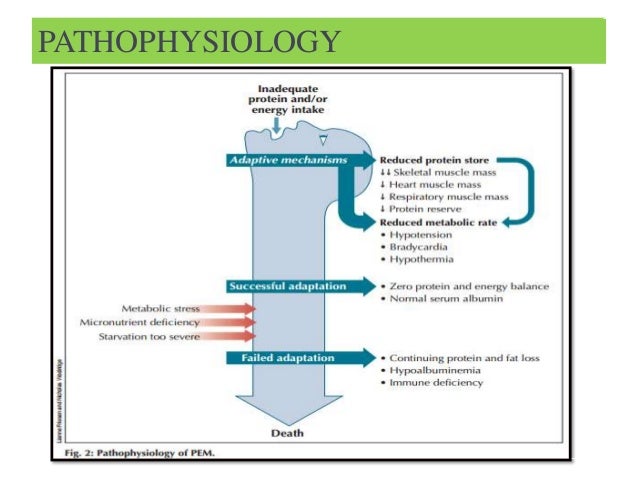
- According to high prevalence of malnutrition in patients with ESRD undergoing hemodialysis, periodic assessment of nutritional status is necessary in them.
- "Meanwhile SGA was found as the best tool to assess nutritional status in patients with ESRD undergoing hemodialysis, because it can recognize various degrees of malnutrition that may remain undetected by a single laboratory assessment."
- "Subjective global assessment (SGA) is a tool used by health care providers to assess nutritional status and aids in the prediction of nutrition-associated clinical outcomes."
- "It is inexpensive and rapidly conducted. Moreover, it has been recommended by the National Kidney Foundation (NKF) Kidney Disease/Dialysis Outcomes and Quality Initiative (K/DOQI) for use in nutritional assessment in the adult dialysis population."
- "Subjective Global Assessment (SGA) is a tool to assess nutritional status that uses
- 5 components of a medical history
- weight change
- dietary intake
- gastrointestinal symptoms
- functional capacity
- disease and its relation to nutritional requirements
- 3 components of a brief physical examination
- signs of fat and muscle wasting
- nutrition-associated alternations in fluid balance"
- "SGA was originally used to predict outcomes in surgical patients; however, its use has gone beyond this function and population."
- "In chronic kidney disease patients, SGA is incorporated into the complete nutritional assessment."

Comments
Post a Comment