80 yrs male with complaints of vomitings 2 episodes since morning and giddiness since morning
80 years male who is a farmer by occupation came to casuality with chief complaints of vomiting 2 episodes since morning and giddiness since morning.
HOPI:
- Patient was apparently asymptomatic 4 years back and on road in village health checkup he was diagnosed to have hypertension and he was put on tablet atenolol 50 mg since 4 years.
- Today morning, he woke up and ate food and after 2 1/2 hours, he went to his work in field, while working in the field he had sudden onset of giddiness followed by vomitings-2 episodes - bilious,non projectile type not associated with pain abdomen, fever, loose stools.
- Vomitings followed by giddiness (self reeling type) since morning - sudden onset aggravated with movements or sitting up, swaying while walking present, associated with headache holocranial type, associated with nausea and vomitings.
- No history of loss of consciousness, seizures, diplopia, blackouts, chest pain, constipation, sweating and palpitations, earache, aural fullness or discharge, tinnitus
- No complaints of weakness, tingling or numbness of limbs, difficulty in chewing, swallowing, deviation of mouth
- No bowel and bladder incontinence.
PAST HISTORY:
- K/C/O Hypertension since 4 years - on treatment TAB. ATENOLOL 50 mg
- Not a K/C/O diabetes mellitus/TB/Epilepsy/BA/CAD/CVA
PERSONAL HISTORY:
Diet- mixed
Sleep- adequate
Appetite- decreased since 10 days
Bowel and bladder movements- regular
No known allergies
- ALCOHOLIC SINCE 40 YEARS- 3 times/week 90 ml
- SMOKER SINCE 40 YEARS- 1 packet/day
FAMILY HISTORY: Not Significant
GENERAL EXAMINATION:
-Patient is Conscious, coherent and cooperative.
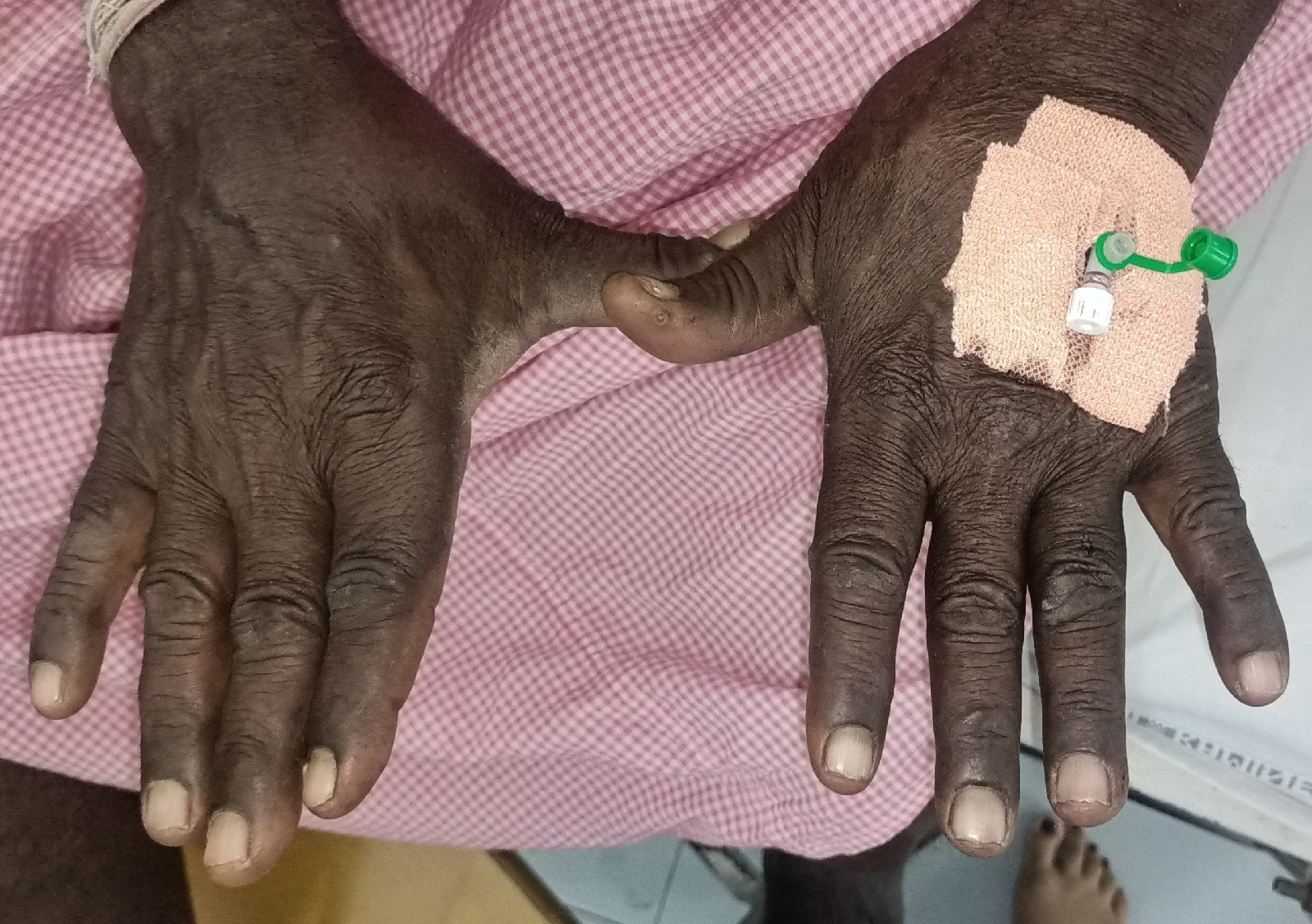
-No pallor, icterus, cyanosis, clubbing, koilonychia, lymphadenopathy, edema.
VITALS:
Temperature - Afebrile
PR- 68 bpm
RR- 14 cpm
BP- 120/70 mmHg
SpO2- 99% at RA
GRBS- 132 mg/dL
SYSTEMIC EXAMINATION:
CVS- S1S2 heard, no murmurs
RS- BAE+, NVBS+
P/A- Soft, Non-tender
CNS:
Patient is oriented to time,place,person
Memory : recent, remote intact
Speech: Normal
Cranial nerves: Intact
Motor system:
Power-5/5 in both upper and lower limbs
Tone- Normal in bilateral upper and lower limbs
Sensory system: crude ,pain, temperature, fine touch, joint position, proprioception are normal in all dermatomes
GCS: 15/15
GAIT:
Reflexes :
Biceps, Triceps, Supinator, Knee and ankle reflexes were absent
Plantars: mute
Cerebellum:
Finger nose coordination +
Knee heel coordination +
No dysdidokinesia.
Nystagmus+ in both horizontal and vertical gaze.
INVESTIGATIONS:
Hemogram on 6/01/2022:
Hemogram on 7/01/2022:
CUE:
PT,APTT,INR:
ECG on 7/01/2022:
ECG on 8/01/2022:
USG ABDOMEN:
MRI BRAIN:
ASSESSMENT:
Giddiness under evaluation secondary to ?PCA Stroke with Hypertension.
ENT REFERRAL:
PLAN OF CARE:
1) INJ. THIAMINE 1 amp in 100 ml NS IV/TID
2) INJ. OPTINEURON 1 amp in 100 ml NS Slow IV/OD
3) INJ. PANTOP 40 mg IV/BD
4) INJ. ZOFER 4 mg IV/TID
5) TAB. PROMETHAZINE 25 mg PO/TID
SOAP NOTES:
7/01/2022:
Day 2
SUBJECTIVE:
No episodes of vomitings
Giddiness reduced than yesterday,but still present
Head ache and nausea
OBJECTIVE:
Bp:120/70mmhg
PR 83bpm
RR: 16
Spo2 :98% at room air
Cvs:s1s2+
Rs: NVBS
Nystagmus +
ASSESSMENT:
PCA stroke with hypertension
Giddiness under evaluation
PLAN OF CARE:
ENT Opinion to be taken
1) INJ. THIAMINE 1 amp in 100 ml NS IV/TID
2) INJ. OPTINEURON 1 amp in 100 ml NS Slow IV/OD
3) INJ. PANTOP 40 mg IV/BD
4) INJ. ZOFER 4 mg IV/TID
5) TAB. PROMETHAZINE 25 mg PO/TID
8/01/2022:
Day 3
SUBJECTIVE:
No episodes of vomitings
Giddiness reduced than yesterday, but still present
Head ache and nausea +
OBJECTIVE:
Bp:150/90mmhg
PR 83bpm
RR: 16
Spo2 :98% at room air
Cvs:s1s2+
Rs: NVBS
Nystagmus +
ASSESSMENT:
Giddiness under evaluation with PCA Stroke
PLAN OF CARE:
1) INJ. THIAMINE 1 amp in 100 ml NS IV/TID
2) INJ. OPTINEURON 1 amp in 100 ml NS Slow IV/OD
3) INJ. PANTOP 40 mg IV/BD
4) INJ. ZOFER 4 mg IV/TID
5) TAB. PROMETHAZINE 25 mg PO/TID
Day 4
ICU Bed-2 case shifted to Ward:
S: Headache + , giddiness +
No nausea, No episodes of vomitings
O:
Pt. is C/C/C
Afebrile
Bp: 120/70 mmHg
PR: 80 bpm
RR: 14 cpm
GRBS-: 109 mg/dL
Spo2 :98% at room air
CVS: S1S2 +
RS: BAE+ , NVBS+
P/A: Soft, Non-tender
Nystagmus +
B/L Plantars: Flexion
A :
PCA Stroke with Hypertension with Alcohol and Tobacco Dependence Syndrome (Chronic Smoker and alcoholic )
P :
1) TAB. PROMETHAZINE 25 mg PO/TID
2) INJ. VERTIN 16mg PO/TID
3) TAB. AMLONG 5 mg PO/OD (8 am)
4) TAB. PANTOP 40 mg PO/OD
5) TAB. AUGMENTIN 625 mg PO/BD
6) TAB. THIAMINE 100 mg PO/BD
7) TAB. NAPROXEN 250 mg PO/BD
8) Vitals monitoring - 4th hrly
10) GRBS 12th hrly
















Comments
Post a Comment