43 year old with LOC associated with tonic clonic movements of hands and loss of memory
43 years old labourer by occupation came with c/o loss of consciousness associated with tonic clonic movements of hands and loss of memory of the episode suggestive of seizure.
No h/o tongue bite, frothing.
Following this episode, she went to local hospital where she was found to have high BP recording and was given TAB. ATENOLOL.
H/o heartburn, regurgitation (burning sensation in throat), dyspepsia, belching , flatulence since 4 years suggestive of GERD.
Currently using medication (ranitidine, aluminium magnesium syrup), domperidone) for the same.
C/O nausea since yesterday.
C/O giddiness since yesterday.
C/O headache (more in the frontal and temporal areas)since yesterday.
She has myopia for which she has been using spectacles (on and off) since last year.
No h/o loose stools, burning micturition.
No h/o palpitations, Dyspnea, chest pain.
No h/o vomitings.
No h/o cold, cough, fever.
H/o fall 20 years ago which resulted in lateral dislocation of left knee. Did not take any treatment for the same.
H/o fall 9 months ago while walking which resulted in fracture of left tibia following which nailing was done.
PAST HISTORY:
Not a K/C/O DM, HTN, TB, BA, Epilepsy, CAD, CVA.
FAMILY HISTORY: Not significant
MENSTRUAL HISTORY:
Hysterectomised 7 years ago in view of fibroid.
MARITAL HISTORY:
28 years marital life, P3L3A1
PERSONAL HISTORY:
Diet- Mixed
Appetite- normal
Sleep- inadequate
B&B habits- regular
Occasional toddy drinker
GENERAL EXAMINATION:
She is conscious, coherent, cooperative, well oriented to time, place, person. She is moderately built and moderately nourished.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, Edema
Vitals:
Temperature- Afebrile
BP-
220/100 mm Hg (on admission)
120/90 mm Hg (14/12/21)
PR- 76 bpm
SpO2- 98% @ RA
Systemic Examination:
CVS- S1,S2 sounds heard
RS- BAE +, NVBS heard
P/A- Soft, non tender, Bowel sounds heard
CNS-
At admission: GCS- E2V3M4
R L
Tone. UL Reduced Normal
LL Normal Normal
Power- Not elicited
Reflexes- Exaggerated Normal
Plantar- Withdrawal Flexor
No signs of meningeal irritation
Cerebellar signs- Not elicited
INVESTIGATIONS:
ECG:
USG Abdomen: shows Grade-I Fatty Liver
CT BRAIN:
Treatment-
1. Inj. LABETALOL 10 mg I.V./STAT
2. TAB. AMLONG 5 mg STAT
3. TAB. PAN 40 mg PO/ OD
4. TAB. ULTRACET
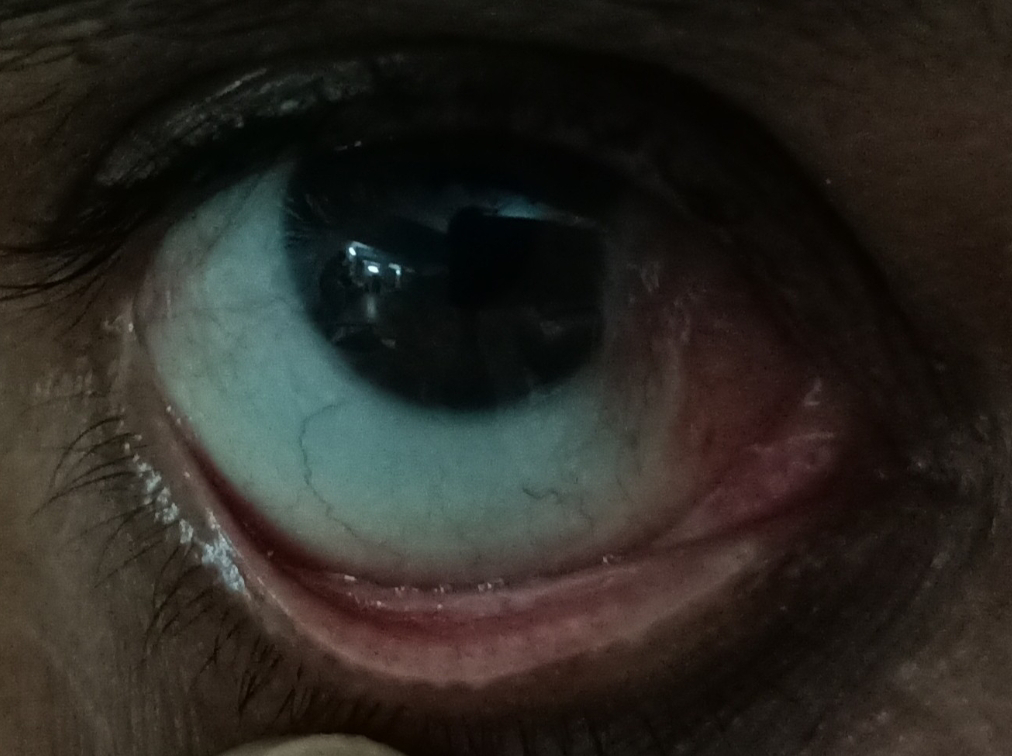
5. Ophthalmology referral was done in order to rule out hypertensive retinopathy
PROVISIONAL DIAGNOSIS:
Hypertensive Urgency













Comments
Post a Comment